Antibiotic Resistance: A Looming Global Crisis
Sir Alexander Fleming, the discoverer of antibiotics, once said,
"This antibiotic will save millions of lives today. But in the future, it will stop working. Millions will die again for trivial reasons."
His prediction is coming true as antibiotic resistance is now one of the biggest global health threats.
Understanding Antibiotic Resistance
Antibiotics must be taken at a prescribed dose and for a specific duration. If not, a phenomenon called "antibiotic resistance" occurs.
Let’s consider a scenario:
Suppose a person has 100,000 bacteria in their body.
The full course of ampicillin (an antibiotic) requires 10 doses to eliminate the bacteria.
However, if the person takes only 7 doses, 70,000 bacteria are killed, and the person may feel better.
But 30,000 bacteria remain. These surviving bacteria adapt and develop resistance mechanisms, such as producing enzymes that deactivate the antibiotic or altering their structure to prevent the drug from binding.
These bacteria reproduce and pass their resistance to the next generations, making them completely immune to ampicillin.
Next time the person takes ampicillin, it will no longer work.
The Domino Effect of Resistance
The problem doesn’t remain confined to one person:
Resistant bacteria spread through sneezing, coughing, and touch, infecting others in the community.
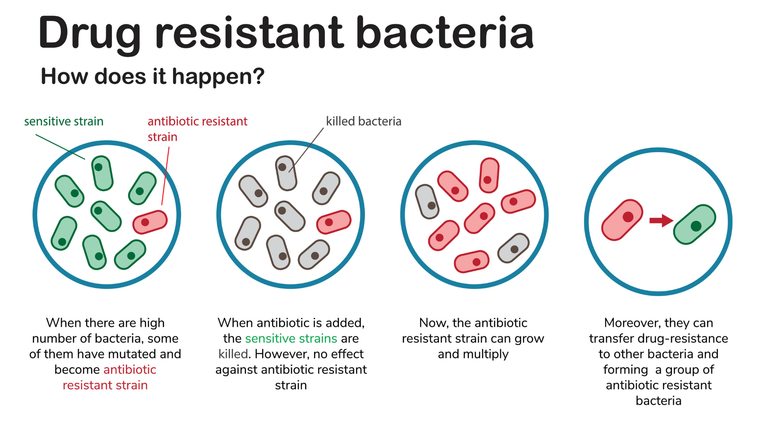
Eventually, an entire region may become resistant to that antibiotic. Even those who strictly follow medical advice suffer because the bacteria circulating in their environment have already evolved resistance.
The Current Global Situation
According to the World Health Organization (WHO):
At least 1.27 million deaths per year are directly caused by antibiotic-resistant infections.
More than 4.95 million deaths in 2019 were associated with antimicrobial resistance (AMR).
By 2050, antibiotic-resistant infections could cause 10 million deaths per year, surpassing cancer.
In South Asia, 70-90% of antibiotics are prescribed or taken unnecessarily, leading to higher resistance rates than in developed countries.

Alarming Antibiotic Resistance Trends in South Asia
The Davidson’s Principles and Practice of Medicine, often called the "Bible of Medicine," specifically mentions the Indian subcontinent in many treatment guidelines, stating:
"This organism is resistant to this drug in the Indian subcontinent."
This highlights the severity of antibiotic resistance in this region.
The Role of Over-the-Counter Antibiotics
One of the biggest reasons for increasing resistance is the unregulated sale of antibiotics in pharmacies.
In many developing countries, patients can purchase antibiotics without a prescription.
A pharmacist or storekeeper, with no medical expertise, often prescribes strong broad-spectrum antibiotics like azithromycin, cefixime, cefuroxime, or levofloxacin.
They tell patients: "Just take one dose, and you’ll be fine."
As a result, bacteria are exposed to sub-lethal doses, accelerating resistance development.
The Future of Medicine is at Risk
Many antibiotics have already lost effectiveness.
New antibiotic development is not keeping pace with the rise of resistance.
Multi-drug-resistant (MDR) bacteria are emerging, where no known antibiotics work.
If this continues, even minor infections will become fatal.
Even if we build modern hospitals with highly trained specialists (FCPS, MD, PhDs), they will be powerless against resistant bacteria.

What Needs to Be Done?
- Strict Antibiotic Regulations
Governments must enforce prescription-only antibiotic sales.
Pharmacies should be penalized for selling antibiotics without proper guidance.
- Public Awareness Campaigns
Media should actively promote rational antibiotic use, just as they do for hand hygiene and vaccinations.
Patients must understand that not every fever requires an antibiotic.
- Improved Medical Education
Doctors should be trained in antimicrobial stewardship.
Rapid diagnostic tests should be used before prescribing antibiotics.
- Investment in New Antibiotics
Governments and pharmaceutical companies must fund research for new antibiotics.
Conclusion
We are heading towards a post-antibiotic era where common infections could once again become deadly.
If immediate action is not taken, the world will face an antibiotic crisis worse than any pandemic.
The time to act is now—before it is too late.
Posted Using INLEO