Why I am hoping for a HOMEBIRTH and why I have made TWO birth-plans:
I didn’t make a plan with my first two births, and our third didn’t go according to plan either.
So fourth time round I have made a detailed birth plan and also a back up emergency plan that I urge every expectant mumma to do too.
Having two birth plans will ensure that my midwife team are aware of my wishes and also should I need to be transferred to hospital that I can hopefully still continue with a ‘gentle’ emergency caesarean.
It is also helpful for my partner follow and , to know what my wishes are, so that he is more relaxed and can enjoy the Birth too.
Having had two natural births and then Bonnie by emergency caesarean some people, including my husband think that I am completely mad wanting to have a home birth.
I used to think this too! Why would anybody want to have a homebirth? when surely the security of the hospital surroundings and knowing a medical team are very close by after having an emergency caesarean would be enough to encourage me NOT to have our next baby at home.
But it is actually reflecting on my previous experience that made me reconsider, research more and feel 100% confident with wanting to birth this baby in the comfort of our own home.
For me, having an emergency C-section came with plenty of negatives – a longer hospital stay, weeks of recovery time, and lifting and driving restrictions. I also experienced the added emotional trauma which has left me quite an anxious person.
In the law of nature when an animal is giving birth, she will go look for a safe space to deliver her young. If she senses any danger or any stress, her labour will automatically slow down and stop until she feels safe again. Its the same with us as humans, if during our precious moment our surroundings feel unsafe, unhappy, uncomfortable or stressed it will only prolong our labour, make dialation slower or even limit our pushing capacity.
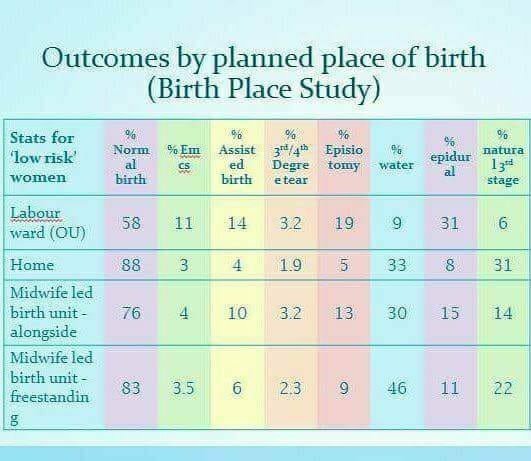
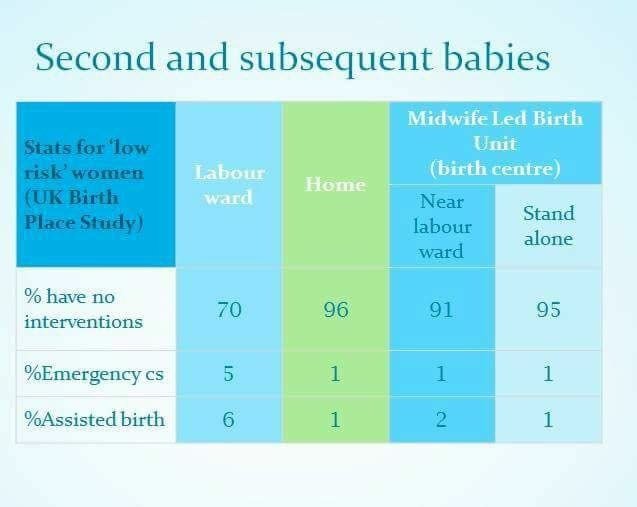
Research shows that caesareans have an increased rate of postpartum depression and anxiety. Hospitals are for the sick and injured, a labouring woman is neither of those. Statistics show that as soon as a labouring woman enters the hospital, the chances of her needing a unplanned caesarean increases dramatically!
(See the screenshot of statistics)
Women who want a home birth are often accused of being selfish and of putting their babies at risk, without any evidence to support these claims. Indeed, research evidence indicates that the health outcomes of planned home birth are as good as or better than those for hospital birth, and that many women experience a range of emotional and practical benefits from giving birth at home.
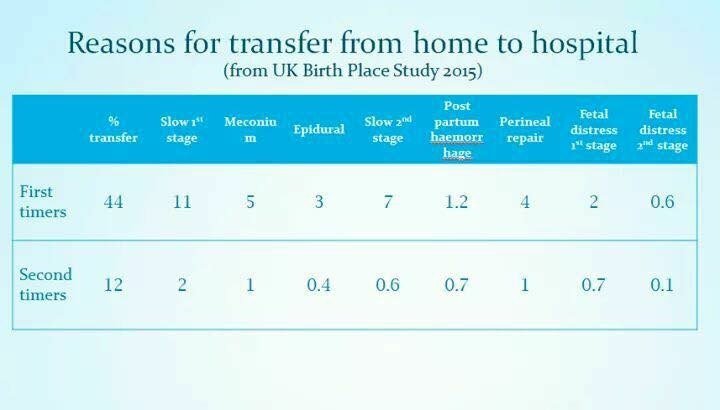
Aside from the way the medication left me feeling after the unplanned section- which was dreadful for weeks! Opting to have a HVBAC will allow me to have a quicker recovery compared to a caesarean. My other main reason for wanting a home birth, is that I need to know that Bonnie (our youngest) is nearby. She is not used to being without me, we nap together bedshare and she still dry nurses. So my mind will be much more at ease and able to focus on the birth if I know she is able to be near me. We also have my very close friend on standby, that Bonnie is used to spending time with, just incase the unthinkable happens and I need to go to hospital.
So my decision to choose a natural homebirth has not been done without reason or research and I am confident that my body is capable of achieving a natural HVBAC.
If I do need to have a Hospital birth. I will be planning to spend most of my labour at home. Just as I did with our second daughter. It is widely accepted that the less time you spend in the hospital, the lower your risk of medical interventions during your birth. Staying home as long as possible is often recommended by midwives, doctors, doulas, and nurses alike.
Of course, the longer you stay home, the closer you are to having your baby when you get in your car, drive to the hospital, fill out admissions paper work and find your room. At this point you are probably / hopefully experiencing strong birth sensations that are coming quite frequently. Usually, all you want to do at this point is stay exactly where you are and focus on birthing.
During a home birth, that’s exactly what you get to do! There is no anxiety about choosing the “right” time to go, avoiding going “too early” or “too late”; you call your support team when you want them to come, and when it is time, they stay with you until you have a baby.
I have made two birth plans. The first being for a successful vaginal HOMEBIRTH and the second being a back up plan should I need to be transferred for an emergency GENTLE CAESAREAN.
What is a gentle caesarean?
A gentle cesarean (sometimes called a family-centered birth) includes many features, but its overall purpose is to invoke a peaceful, calm atmosphere that closely mimics what happens during and immediately after a natural childbirth.
Michelle’s VAGINAL HOME BIRTH Plan (A)
BEFORE LABOUR BEGINS:
- I would like a homebirth by vaginal delivery and will labour at home for as long as possible unless an emergency and I need to be transferred to hospital.
- As long as the baby and I are healthy, I would like to go at least 10 to 14 days over my due date. If I go past my due date and the baby and I are fine, I prefer to go into labor naturally rather than be induced.
- As long as the baby and I are healthy, I would like to have no time restrictions on the length of my pregnancy.
FIRST STAGE OF LABOUR:
- I do not want any vaginal examinations. Please use alternative methods to check for dilation - please see full details below (* Mexican Hot Legs, Check Mums Breathing and Behaviour)
- Should a vaginal examination be required, I prefer not to have my membranes broken unless there is an emergency situation
- Please only suggest pain management options for me if you see that I am too uncomfortable to handle the pain. I wish to use Breathing techniques, Visual imaging, bath/shower, walking, yoga, homeopathic remedies, clary sage essential oil massage.
SECOND STAGE OF LABOUR:
- As long as the baby and I are healthy, I prefer to have no time limits on pushing.
- I want to be able to move around as much as possible, rather than lying flat on my back.
- I prefer to have no episiotomy and risk natural tearing. No vacuum or forceps (unless a medical emergency)
- Please encourage me to breathe properly for slower crowning.
- If possible, please allow the shoulders and body of my baby to be born spontaneously, on their own
- I will eat a couple of dates to help soften my cervix and reduce bleeding after birth
THE DELIVERY:
- I would like to touch my baby's head as it crowns.
- I would like me or my partner to catch the baby when born and place baby straight onto my chest without any rubbing or cleaning of the baby. Please leave all of the vernix on my baby. Full skin to skin contact with a blanket over baby for at least an hour.
- No hat or mittens to be placed on the baby after birth.
- Please delay all essential routine procedures on my baby until after the bonding and breastfeeding period
- I would like for our baby to hear our voices first.
- I prefer to have the lights dimmed for delivery or, if it is daylight, to access only natural light.
- It's important to me to push instinctively. I would rather not be told how or when to push.
- Please do not separate me and my baby for newborn procedures (weighing etc) until after my baby has successfully breastfed on both breasts.
THIRD STAGE OF LABOUR:
- Please wait for the umbilical cord to stop pulsating before it is clamped (at least 20 minutes or longer if I wish)
- Please help my partner to use the umbilical cord tie that we provide (rather than the plastic clamp)
- I would prefer for the placenta to be delivered spontaneously without the use of pitocin, and/or controlled traction on the umbilical cord. The placenta will deliver using natural oxytocin through breastfeeding and skin to skin contact with my baby. If necessary I will use my homeopathic remedy to help deliver the placenta.
- Cord blood to be tested to determine babies blood group as to whether I will need the Anti D injection.
- I will have eaten a couple of dates during labour to help reduce bleeding and also have a homeopathic remedy should I need to use it. However will discuss any medical reasons that I may need medication to stop haemorrhaging.
- If me or the baby has any problems, I would like my partner to be present with the baby at all times, if possible. I would like to have routine newborn procedures delayed until bonding and breastfeeding have occurred. I would like all newborn routine procedures to be performed in my presence, baby not to be taken from my sight.
- We decline any form of Vitamin K to be given to the baby (unless a medical emergency, at which time we will discuss if necessary)
Michelle’s GENTLE EMERGENCY CAESAREAN (PLAN B):
My natural birth plan to be followed as closely as possible. But should I need to be transferred from home to hospital for an emergency caesarean:
- I would prefer an epidural or spinal block rather than general anaesthetic unless a medical emergency requires me to.
- Please do not automatically give me extra drugs to relax, so that I can be fully present for the birth experience
- Partner to be in the operating theatre at all times.
- If I cannot be conscious, father (my partner) should be allowed to hold our baby skin-to-skin immediately after birth, barring any medical complications with baby
- Please do not clean or wipe the babies vernix
- Minimal handling of baby before passing to me (or if not possible, baby to have immediate skin to skin with my partner)
- If me or baby have any monitoring devices attached, please can they be placed in areas that don’t infringe my ability to see, hold or breastfeed my baby
- My theatre gown to be lowered and baby can be placed immediately on my chest while I am being stitched. To facilitate this, please ensure my arms are not strapped down
- Baby to breastfeed immediately while in the operating room
- Please ensure of Delayed cord Clamping for at least 20 minutes or at least until the cord stops pulsating.
- Partner to cut the cord and help use the umbilical cord tie (rather than the plastic clamp)
- No hat, clothes or mittens to be placed on baby. My partner (baby’s father) will help dress the baby when I am ready to part with baby for a short while.
- Cord blood to be tested to determine babies blood group as to whether I will need the Anti D injection
- Lights as dim as possible for a calm environment for our baby.
- Any usual post-birth procedures such as weighing the baby are delayed until I feel me and baby are ready and baby has successfully fed from both breasts.
- We decline any form of Vitamin K to be given to the baby (unless a medical emergency, at which time we will discuss if necessary)
- Doctor to do a vaginal swab to give the baby the best microbiome possible (**see details below)
- Baby to stay with me at all times after delivery.
- I would like to safely bedshare with baby rather than be placed on a bedside cot
- I would like to leave hospital as soon as possible following the birth.
- Should I need to stay in hospital for longer than 24 hours, then I would like to be transferred to a private room where my partner can stay too. We will pay privately to do so if there is availability of such a room.
- All siblings of new baby to be allowed to visit at any time.
POSSIBLE INDUCTION:
- Should I go over my due date , I would like to try natural induction methods before discussing medical intervention.
- I would still prefer a VBAC should I go over my due date, unless there are any medical reasons preventing me to.
*Alternative to vaginal examination
- Mexican Hot Legs
Providing mum is on dry land and not in the birth pool and she does not have a temperature). Check if the leg is warm but only the feet and ankles are cold, a woman’s cervix is generally about 3cm dilated, if she is cold up to a little higher up the leg to mid-calf area, around 5cm, and if the entire leg up to her knees is cold she will be fully dilated and ready to push very soon. The reason for this is that blood flow gradually decreases to the extremities as labour progresses because it is needed higher up in the body. - Read mums breathing and behaviour
The pitch of her voice, and how she is moving around should also be clue enough as to how far a woman is dilating.
** Vaginal Swab after caesarean
When a baby goes through the birth canal during a vaginal birth, he or she is exposed to a plethora of microbes – in baby’s mouth and on the skin. These bacteria help build a healthy microbiome for your baby, which could reduce his or her risk of inflammatory illnesses like Crohn’s disease, heart disease, infections, and much more.
With a gentle caesarean, your doctor or midwife can collect a vaginal swab and wipe it on your baby’s skin and in his or her mouth to contribute toward a positive microbiome. Another option is to take a swab of your vagina and wipe it on your nipples before baby breastfeeds.
@allthingsbabyandme
Please feel free to copy any sections or the whole of my birth plans.
Remember to print lots of copies off and keep one in your handbag, with your midwife, birth partner, in your car, in your birth notes etc.
Here is a list of my relevant blog links that you may find interesting regarding any of the above points:
No Vaginal Examinations ~
bit.ly/2OLLVUq
No Vitamin K ~
bit.ly/2Ba6Xs9
Third stage of labour (delivering the placenta without pitocin)
bit.ly/2zTYCqz
The Importance of Delayed Cord Clamping:
bit.ly/2A10EVU
Natural Homeopathic Remedies for pregnancy, birth and beyond:
bit.ly/2Q2Io8I
Why you shouldn’t put a hat on your newborn straight after birth:
bit.ly/2QM1sp0
Preparing My Home Birth Box and Emergency Hospital Bag:
bit.ly/2zbA5O8