Sharing some images of malignant cells and highlighting the common stuff we always look out for. Here's some pics from a gallbladder aspirate suspected to have adenocarcinoma.
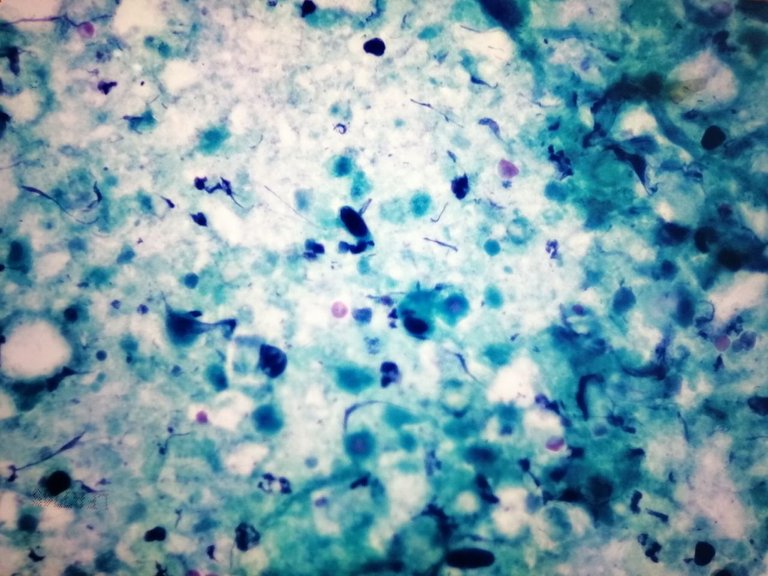
Just from low power, you can spot odd clusters of suspicious cells based from size.

Mitosis admixed in a background of necrotic debris.
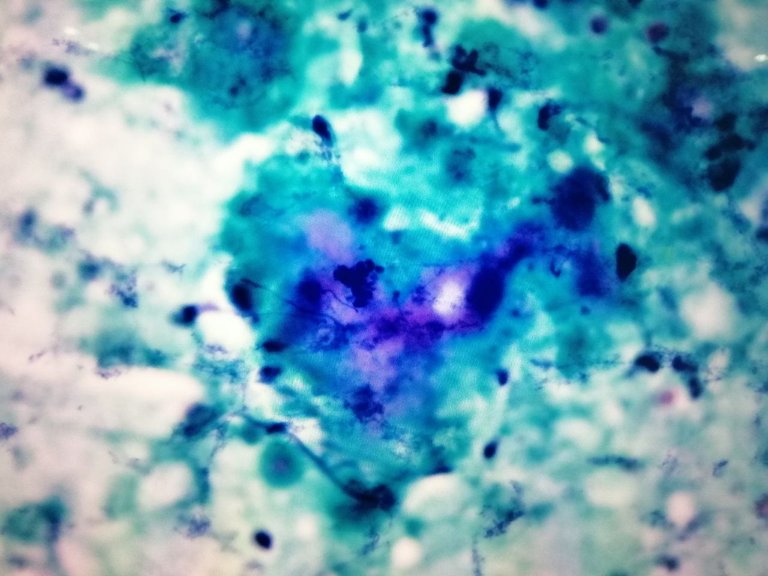
Some of these cells are normal and some have rather relatively large nuclear membranes and darker chromatin compared to their neighbors.
Nuclear pleomorphism.
If the nuclear membrane doesn't look regularly round and vary in size in relation to other cells of it's lineage. An irregularly shaped nuclei compared to its neighboring cells triggers alarms.
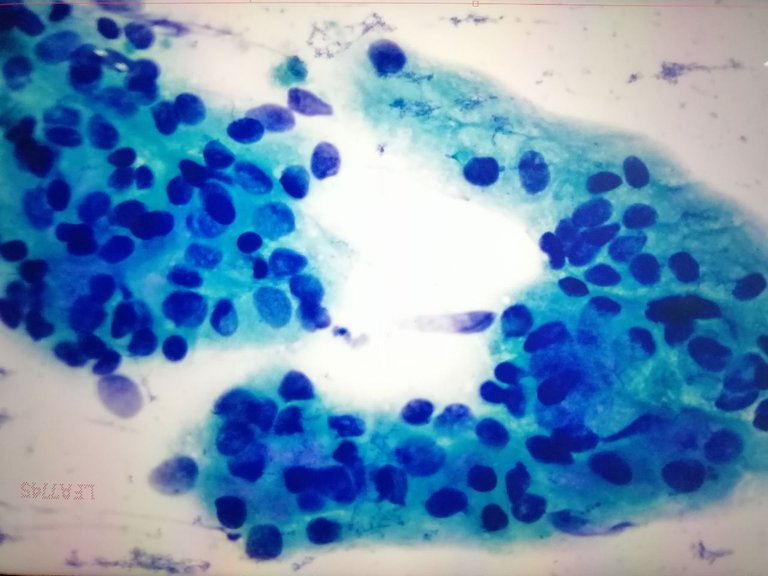
Mitosis
Mitotic figures plus pleomorphism are solid indicators. You don't usually see mitotic figures on most specimens recovered during smears.
Necrosis as a background.
The presence of dead cells, inflammatory cells and abscess indicates that there is something wrong unless there is confirmation that the site where the specimen was taken from does have abscess. But a sterile site presenting with necrotic debris rings alarms. Sometimes, specimens without necrosis and inflammatory cells helps highlight the tumor cells. Inflammation can sometimes make normal cells reactive which can confuse the observer to mistake them for malignant cells.
Circumstances that help us figure whether it's malignant versus normal:
Location where the specimen came from.
If you see the type of cells that aren't supposed to be there, suspect it may be a wrong specimen label or probably metastatic.
History.
If the patient has an established history of malignancy, then the type of cells we're looking for gets easier to ID. This also helps rules out suspicion of other suspicious cell with similar morphology. The clinical diagnosis of the patient also helps to narrow down benign versus malignant cases.
Timing.
Pap smear specimen can change based on the type of cells predominate during the time of collection. Knowing the patient is pregnant, taking contraceptives, or timing of the menstrual cycle helps explain the predominance of this specific cells on the smear.
And lastly, different specimens would require different adequacy criteria. It's not enough that we have a scant sample, the sample must contain x number of cells on the smear to ensure we're getting as close to the accurate representation of the disease. You can't really say malignancy is ruled out if there isn't enough cells present to examine. Sometime there's no consensus as to how much should be present because different societies have different recommendations and the guidelines will depend on what the empirical research published so far.
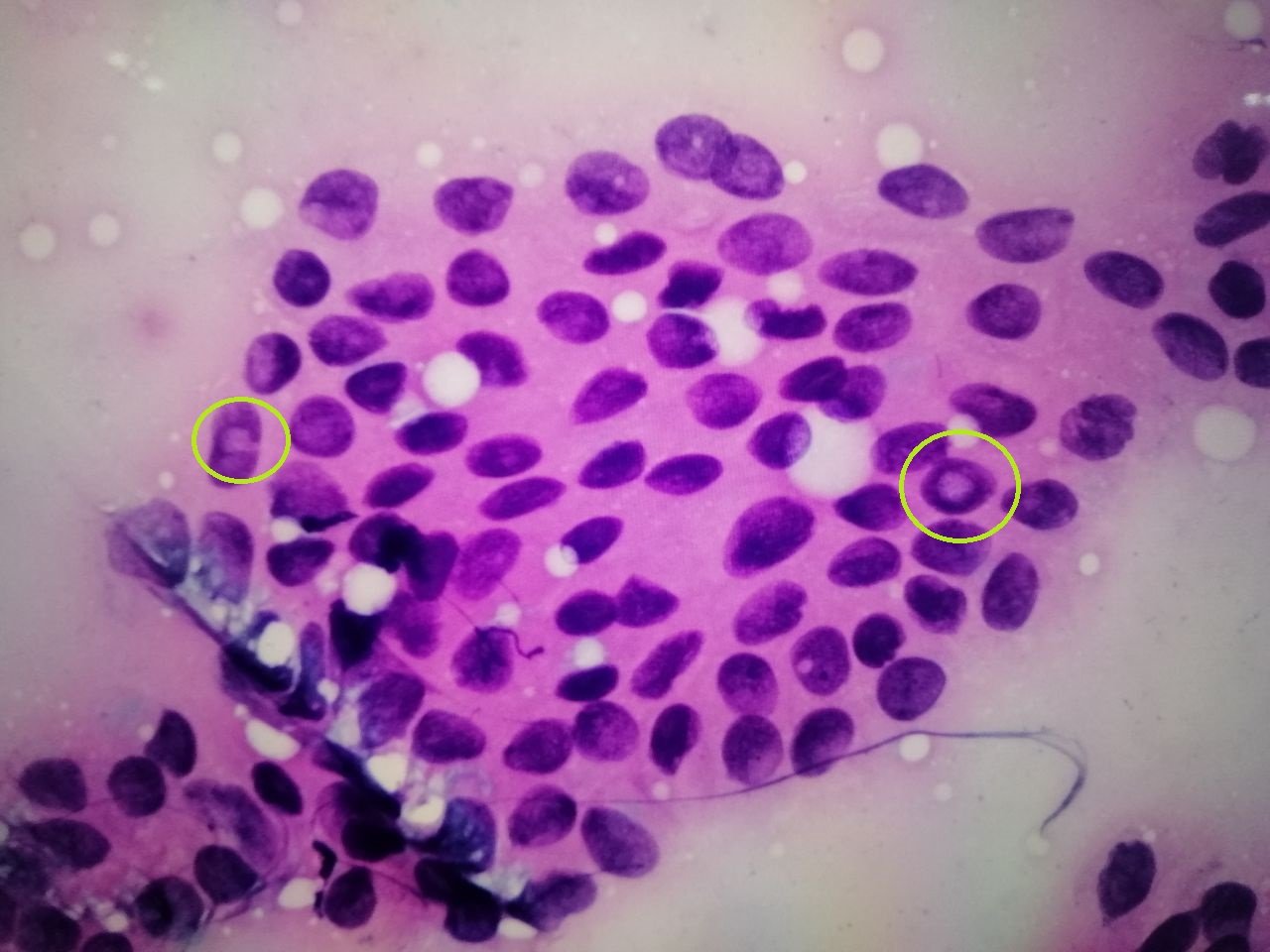
An old pic of a papillary thyroid carcinoma suspected case based on cytology alone.
And a cluster of malignant cells from pleural fluid.

So even if I don't know the site where the specimen was taken and I'm just looking at the smears without prior knowledge of the history, the above features mentioned are the ones I'd need to look out for because these three things present at once can help me clinch the diagnosis.
If you made it this far reading, thank you for your time.
Posted with STEMGeeks