Hello,
And welcome to my blog, as we continue to battle this virus all across the globe I would like to remind us all that it is incumbent on us to protect ourselves, our families and our neighbors by continually adhering to the protocols put in place to protect us and keep us safe. This too shall pass.
Today I want us to take a look at another condition which is classified under the geriatric category. Age-Related Macular Degeneration is a potential sight threatening condition which affects our central vision and in severe cases render us blind.
Introduction
We may consider Age-Related Macular Degeneration as a progressive disorder of the retina. It is commonly seen among western and eastern descends. Prevalence among Africans is quite low. There is a good chance that individuals diagnosed with AMD may have the case worsening within the next 5 years should it be taken for granted.
The Retina is one of the most active tissues within the human system, some may even consider it as the most active because of which it undergoes lots of work to release energy. In the process of respiration we come to understand that the system is imperfect and so we end having some free radicals here and there, some particles escaping the process and some fat accumulations every now and then.
In the case of the retina these particles sometimes get deposited behind the retina at the area of the macular and accumulate over the years forming what we call drusen. This raises the macular area and impede it function. Sometimes this causes fluids to leak into the macular area causing what we call wet AMD. It is a more severe version of the condition and causes visually loss quickly. When drusen is caused by fats and other particles deposit we get dry AMD. Signs of AMD may start to manifest from the age of 40.
Causes and Risk Factors
Since we have already established that the condition is a geriatric case we can confidently say that age is a risk factor. We also learnt in the previous paragraphs that some races may be more susceptible than other. Aside these habits such as smoking and high fat diet may contribute to one developing AMD. Individuals with cardiovascular conditions such as hypertension may also be at risk.
Diagnosis and Treatment
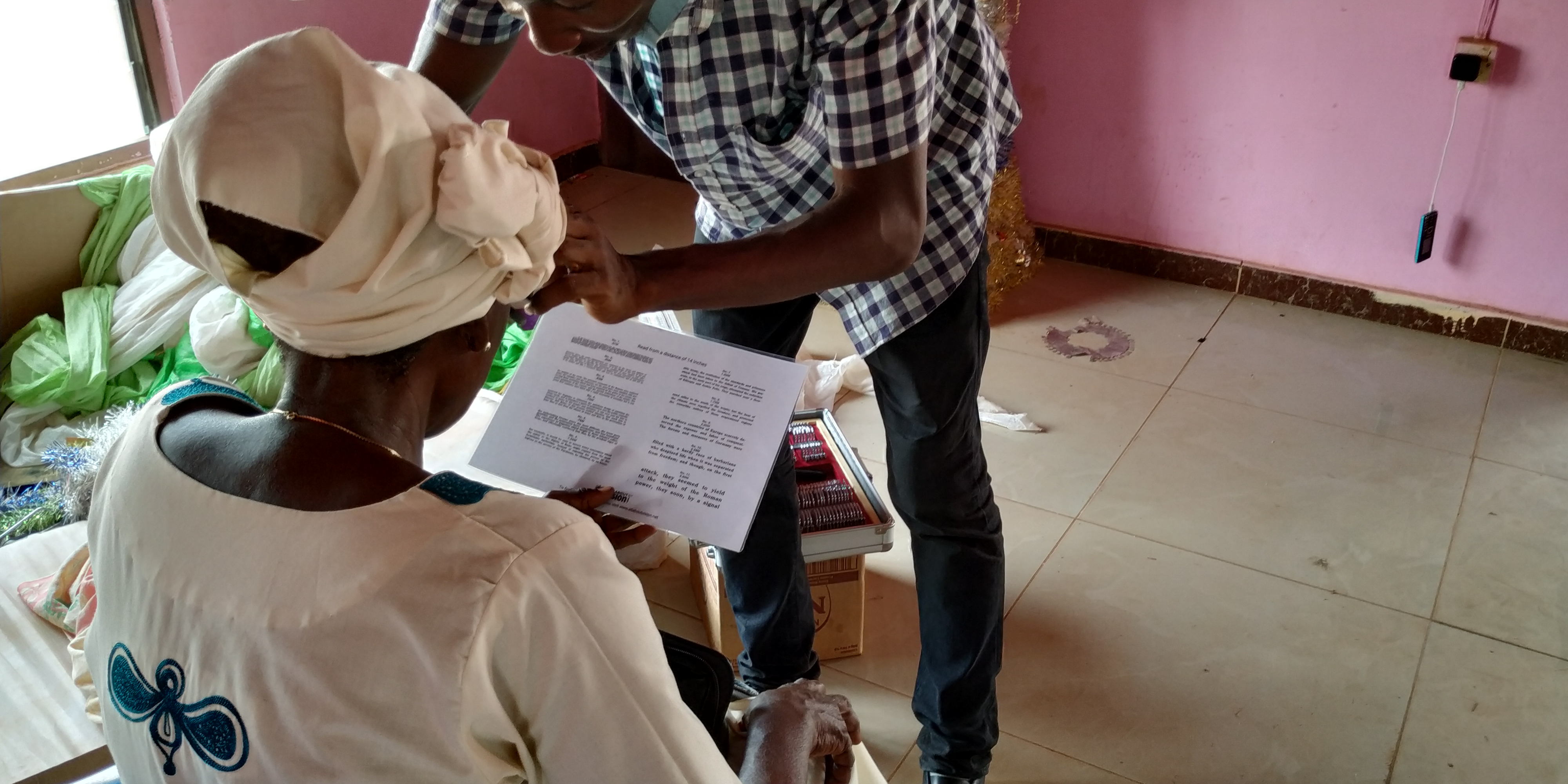
Diagnosing of AMD may initially involve a simple visual test using the Amsler Grid where patient would be required to report any anomalies in the grid appearance such as distorted lines or missing parts. Further test may include angiography and ocular coherence tomography test to ascertain the type and the extent of damage.
One of major treatment methods used is antioxidant supplementation. With no cure in place for AMD we seek to manage the condition and high antioxidant supplementation may help reduce the progression of the condition giving the patient more time to ensure the vision as they may be at the time of diagnosis. Some patients may also require visual aids to help with their vision.
Conclusion
AMD diagnosis is not a blindness sentence however early diagnosis help with a better prognosis for treatment and maintaining or managing vision. Hence, regular eye exams should be practiced, we should not visit the clinic only when we have a problem with our vision because sometimes it may be too late. A healthy diet is a healthy living, good habits should help improve your overall health. Stay healthy and stay safe.
Thanks for reading and have a great week, Special thanks to my mentors and supporters @mcsamm, @tj4real, @armandosodano, @delilhavores, @gentleshaid, @agmoore. For further reading;
Lim, L. S., Mitchell, P., Seddon, J. M., Holz, F. G., & Wong, T. Y. (2012). Age-related macular degeneration. Lancet (London, England), 379(9827), 1728–1738. https://doi.org/10.1016/S0140-6736(12)60282-7
Al-Zamil, W. M., & Yassin, S. A. (2017). Recent developments in age-related macular degeneration: a review. Clinical interventions in aging, 12, 1313–1330. https://doi.org/10.2147/CIA.S143508
Nowak J. Z. (2006). Age-related macular degeneration (AMD): pathogenesis and therapy. Pharmacological reports : PR, 58(3), 353–363.
Gil-Martínez, M., Santos-Ramos, P., Fernández-Rodríguez, M., Abraldes, M. J., Rodríguez-Cid, M. J., Santiago-Varela, M., Fernández-Ferreiro, A., & Gómez-Ulla, F. (2020). Pharmacological Advances in the Treatment of Age-related Macular Degeneration. Current medicinal chemistry, 27(4), 583–598. https://doi.org/10.2174/0929867326666190726121711


Hello @nattybongo,
Another practical blog, with bad news delivered gently. There is always hope in your blogs, encouragement to seek treatment.
My mother had macular degeneration, the wet kind, so it was not a very pleasant course for her. She was diagnosed in the early 1970s and no treatment was offered. She was told to wear very dark sunglasses and to avoid bright light.
I know this condition can be familial, but so far there are no signs of this in me or any of my siblings. I am ten years older now than she was at time of diagnosis.
Thank you for this responsible overview of a very serious condition.
Stay well,
Regards,
AG
Hello @agmoore,
It is always a pleasure to hear from you, you do take you time to read and always share what you got from my writeup. Thank you for reading, and as i always say please do well to have regular eye checkups because prognosis of any condition is better when detected early. I am however glad to hear that all is well for you. Do stay safe and have great week.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider supporting our funding proposal, approving our witness (@stem.witness) or delegating to the @stemsocial account (for some ROI).
Please consider using the STEMsocial app app and including @stemsocial as a beneficiary to get a stronger support.