Arriving at my 20 week antenatal appointment, I was already as anxious as could be. I was approaching the point in my pregnancy where I had learned that my precious boy had passed away, only 12 months before. This time everything seemed to be going well, but I was preparing myself to hear the worst.
My midwife, Michelle, knowing my history, was quick to grab the doppler and lay me on the bed. My heart was beating so hard that when she placed it on my stomach, that was all we could hear. After a few moments of searching, I heard it! It was the most amazing sound! My baby...
A fortnight came and went, and before I knew it, it was time to go back for my next check up. Michelle, being the fantastic midwife that she is, was seeing me fortnightly, keeping a close eye on baby and myself. As usual, she asked questions, felt my tummy and took measurements. This time the news wasn't so great... My belly hadn't grown... Michelle, trying not to worry me, explained that it could be the way the baby had positioned itself, but decided to send me for a scan just to be sure.
I returned to Michelle a week later to get my scan results. Unfortunately, the news wasn't what I had hoped. Not only was there a hole in my baby's heart, but she was really struggling to grow. She was diagnosed with Early Onset Intra-Uterine Growth Restriction or IUGR. This required a referral to the Fetal Diagnostic Unit at the Monash Hospital in Melbourne, where they deal with all the high risk pregnancies.
With in a week, I found myself nervously awaiting my name to be called, for yet another growth scan, but this time with 'the experts'...the best of the best.
Up until this point, I had been dealing okay with the whole situation. The scan was going well, blood flow was looking good, baby was looking healthy, just small. Really small. She was measuring 4 weeks behind. The Dr was fantastic and explained the situation, answering all my questions. The scary part was when she told me that they would be aiming to keep baby inside until HOPEFULLY 32-34 weeks gestation. I left feeling pretty good, everything was well at this stage. I just had concerns about the whole 'hopefully 32-34 weeks' thing. That's early, but more so when she may only be the size of a 28-30 week baby.
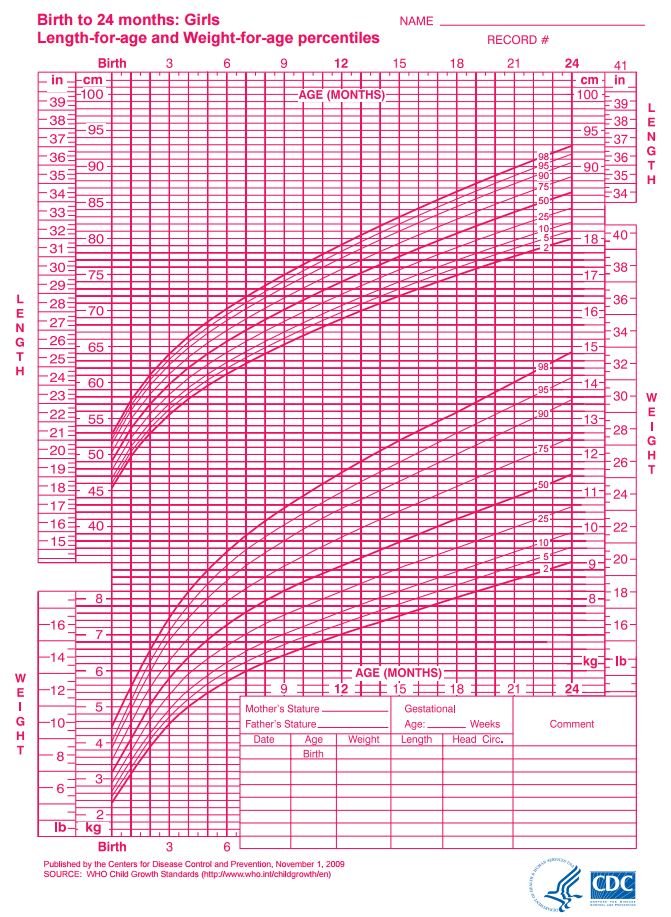
From then on, each week, I would put my hospital bags in the car and set off to Monash for more scans and check-ups, never knowing if they would let me leave after my appointment or if they would admit me, due to changes in the babies environment. At every growth scan I would watch the screen intently, waiting to see or hear if my baby had grown in that fortnight. She was growing, but only just. Each time she would fall further and further behind, or lower and lower on the percentile charts, starting off at around 9%, then falling to 6%, 5% and finally to 3%.
Percentile chart taken from the WHO website. (The average baby is born around the 50th percentile, about 3.5kg. The largest baby is the 100th and the smallest baby is the 1st)
I was beginning to panic as 32 weeks was approaching fast, and with her weight increases declining with each scan, I knew that delivery could be an option at any time - more so than it was before.
I was scheduled for my 32 week growth scan at 32+1. Tears were welling in my eyes as I realised that she had only put on 42 grams in the last 2 weeks...I knew this was not good news. After the obstetrics team had a meeting, they informed me that delivery was not the best option yet, as she was not in immediate danger and required more time for her lungs to develop. And while hearing that was like music to my ears, I was left with strict instructions to make contact with them if baby's movements decreased or if I felt anything was wrong, which came with a huge emotional toll for me.
I had lost my previous baby, but I didn't even know. I didn't feel him kick. But I thought I had. How was I to know if something was wrong. I spent most days over analysing every movement, or every moment with out. What would happen if she did pass away and I didn't know. Would my husband get angry at me for not knowing? Would my family blame me for losing a second child? The thoughts and emotions that come with the death of a baby are indescribable...nothing like I would have imagined. How would it be different this time? How could I tell my husband that he had to bury yet another child? How was I going to explain it to my 5 year old? How would she cope? She's already been through too much, losing her Poppy and her little brother. She was so excited to be getting a baby, especially a sister!
34 weeks came and I met with my team of doctors. The growth scan suggested that she had stopped growing completely. Her abdomen was tiny. She had began 'brain sparing'. This happens when a baby is growing and it can not get enough nutrients to grow fully, so it will send all its nutrient intake to the brain, the most important part, resulting in an abnormally large head with smaller torso and short limbs. Once again, the team had a meeting to discuss where to go from here, and they again decided to let me go another week for lung development. I was to meet them again in a week to discuss delivery plans.
The following week, in I went again. This time I left with a delivery plan. I was to come in 2 days later to begin the induction process. I was warned that there was still a high chance that her lungs wouldn't be developed fully and that she would require help to breath. They also suggested that, due to her size, she may not feed well or grow and may be in the NICU (Neonatal Intensive Care Unit) for some time. This also left me with many questions about hers and my family's future.
How long would she be there? How would I cope leaving the hospital without her? How would my husband cope with working and not having much time to see her? How would my other kids cope not having me there? How would I split my time between them all? How would they cope not being able to see their little sister? How could I afford the costs involved? How was this going to impact my family?
All questions aside, it was what had to be done. So, at 36 weeks gestation, on Tuesday the 22nd of December 2016, at 3pm, I was admitted to Monash Hospital in Clayton, Melbourne to start the induction process. At 6am the following morning my waters were manually broken and a drip was started. I had a long day ahead of me and little did I know, it was going to be full of ups and downs, laughter and tears, beeping of machines and constant monitoring. I had a midwife beside me at all times, watching the baby's heat rate. With each contraction her heart rate would decelerate more and more until I had a team of doctors there, poking, prodding, inserting IV lines, and taking bloods from both me and the baby. When I realised they were preparing to take me to theatre for an emergency c-section, my heart sank. I was scared. I was crying. I just wanted my baby in my arms.
I'm not sure what happened in the next few moments, but suddenly everything stopped. My contractions stopped, the beeping stopped, her heart rate returned to normal and all the people that I had surrounding me had left the room. I was given some medication for the pain, as much as I didn't want it, they insisted I needed to rest. By this time it was 29 hours since my labour had begun.
Between contractions I dosed, not really aware of what was going on. I could feel them finally getting stronger and more frequent. I woke with one almighty contraction, and realised 'this is it'. The midwife checked and sure enough a head was visible. She ran out the door and got the doctors. Once again, I had a room full of people...2 midwives, 4 doctors, a student doctor, a crash cart and no husband.
Two pushes and a total of 6 minutes later, my baby girl arrived. My daughter was finally in my arms. It felt like a life time of whacking her on the back before she finally gasped that first breath and let out a huge cry....It wasn't until I looked at her discharge papers that I realised it was nearly a full 2 and a half minutes before she started to breath, no wonder it felt so long!
Although I knew our journey was not over yet, really, it had only just begun, I felt all the stress and anxiety wash away. My baby was here, she was breathing and she was with me. We were taken to the ward where she was weighed and measured etc. Mini sure was mini! Born under the first percentile at 2.2kg and 40cm long, she was a little doll.
For the next two weeks we had struggles with her weight, feeding, temperature, blood sugars, jaundice and liver problems, requiring intensive phototherapy, until they decided to admit her to the Special Care Nursery and discharge me. Leaving her there was one of the hardest things I have ever had to do. The feeling was unlike anything I had ever experienced before. I needed my baby with me, I needed to be there for her.

Mini sun baking at 3 days old (photo-therapy)
After days and days of blood tests, liver and brain ultrasounds, sugar tests, feeding tests, etc, her liver function began to normalise, allowing her to put on weight 3 days in a row. Her jaundice settled and she began feeding better. It was time to come home!
Where are we now?
Mini is 7 and a half months old now. Since we came home there has been many ups and down, a tonne of appointments and so much love! We have been able to escape any hospital admissions, although we have had a few trips to the E.R. for hypothermia and gastro. Her liver is still being monitored, but is getting better and better each time. Her cardiologist is happy with her heart and feels that the hole is closing over. Her dietician is happy with her weight gains now, although its been very up and down. Her paediatrician is generally happy with how she is coming along, we are just needing her to grow a bit more, as she is still about the size of a 3-4 month old. We aren't completely out of the woods yet.
In the way of IUGR babies, we escaped most of the serious consequences. We were and are VERY lucky. There have been many babies born with IUGR/SGA that have not done well. There were many mothers that were admitted and delivered weeks before me, and their babies were still in hospital weeks after Mini. There will be some that come home with feeding tubes and CPAP machines for breathing. There will be many that never come home.

Mini the day after coming home at 4 weeks old VS. Mini now (Doll 38cm long)
Do you know anyone who has experienced IUGR? How are they doing now?
Comment, up-vote and resteem!
@mel.jai I hope u will get cute baby!!