
Welcome to the very first episode of my newest series, the Pathological rashes of the human body series where we take a look at some of the most precarious yet seemingly innocent or downright conspicuous rashes erupting from the surface of our skin and since the title specifically mentioned the word 'Pathological', the rashes we're looking at are those that accompany a sinister or morbid diagnosis.
Without further ado, let's dive right into it shall we?
Enter Salmon Pink Rash
As tasty as that sound, it's not something you want to see appearing on your child's skin anytime soon.
And Yes, Your child.
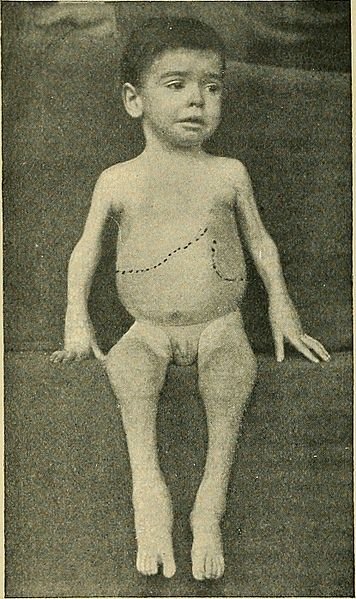
Why the paediatric population? That's because Salmon pink rash is one of the many feature of a paediatric rheumatological condition known as Juvenile Idiopathic Arthritis or JIA but before we dive deeper into the disease, let's study the rash so to help you recgonise it.
HOW IT LOOKS LIKE

As the name suggest, the colour is somewhat similar to that of the pinkish juicy Salmon meat (Yummy). Now, unlike viral exanthems (viral rashes), the Salmon pink rash is nonpruritic in nature (not itchy) and typically appears over the trunk or the extremities during the febrile phase (when fever ensues). The relationship between the rash and body temperature is an interesting one - the rash comes and go according to the variations in temperature which means that during febrile phase, the rashes would be markedly visible and would subside as the temperature go down. Albeit unclear, the best explanation to this relationship is thought to be due to the underlying immune-mediated reactions in the body and slightly similar to the koebner's phenomenon, these rashes may even feel hotter upon palpation or become worsen at sites where there was previously trauma/scratches.
Now that you've indentified the rash, it's time to learn about the diagnosis.
This rash is one of the classical feature of Juvenile Idiopathic Arthritis (JIA). Now, a few things to clarify:
When I mentioned one of the classical feature.. it means that the presence of the rash doesn't necessarily mean that the person has JIA, rather a suggestive feature in combination with other important symptoms such as Extremities pain, Knee pain and swelling, Other chronic joint pain, limping and Red eye.
The name Juvenile Idiopathic Arthritis is pretty self-explanatory as the the disease is a rheumatological condition of unknown etiology affecting the paediatric population and it comprises a few subgroup based on the presenting symptoms.
That said, such rash warrants a visit to the nearby doctor especially if the child has fever because even if you got the rash wrong, a febrile child with rashes should be investigated for other causes.
ABOUT JIA
Previously known as Juvenile Rheumatoid Arthritis (JRA), it is the most common chronic paediatric rheumatological condition affecting about 1:1000 children. The disease has two peaks (at the age of 1-3 years and between 8-12 years) but it can, and it does, occur at any age in the paediatric age group. The common underlying manifestation of JIA is almost always Chronic synovitis (Inflammation of the synovial membrane/synovium). Following the inflammation, the lymphocytes infiltration causes the thickening and hypervascularity of the the synovium which can be proven from the evidence of inflammatory cytokines and lymphocytes in the synovial fluid.
On physical examination by the doctors, typical signs of inflammation is present such as joint tenderness, erythema (redness) and effusion (basically swelling). It's worth mentioning here that JIA is a diagnosis of exclusion, meaning that only after you have successfully and confidently excluded other potential diagnosis, you can say that the likely condition is JIA. That said, the diagnosis is essentially clinical and that further markers or investigations are only supportive.
Classification
There's 2 parameters to look at to classify the different subtypes of JIA.
The first one is based on the number of joints involved with the cut off point being either less than 5 or 5 or more affected joints.
The second aspect is to look at whether the disease presents itself with systemic manifestation or involvement of the sacroiliac joint.
If less than 5 joints are affected, the disease subtypes is known as Oligoarticular. In this group, type of joints involved are usually the medium to large joint such as the knee and elbow with the gender predominance being the female. The incidence of Uveitis is the highest in this subtype but the good news is that this subtype (compared to the other 3) has the best prognosis with more 90% will achieve remission.How it sets itself apart from other subtypes in terms of investigation is that it is the only one that yields positive Anti-Nuclear Antibody (ANA), a common marker tested in ruling out rheumatological condition.
If 5 or more joints are affected, it falls into the Polyarticular subtype with the joints affected are primarily the small to medium joints with (usually) symmetrical arthritis. This account up to 40 of all cases of JIA and in contrast to the previous group, this subtype can also present with systemic inflammation such as malaise, growth stunting, fever, chronic anaemia and sustained elavation of inflmmatory markers (ESR or CRP). How it sets itself apart from other subtypes in terms of investigation is that it is the only one that yields positive Rheumatoid factor.
In around 10% of JIA, the presentation is preceded with systemic manifestation rather than arthritis and this subtype is known as the Systemic-Onset JIA. They typical manifestation of this group is Recurrent, spiking fever averaging once or twice a day with, as you've guessed it, the accompanying Salmon-pink rash. This subtype is particularly interesting to me as a medical student because when synthesising the differential diagnosis for Hepatomegaly (Enlarged liver), you can say JIA as this subtype presents itself with such sign.
In a large gene-association study in 2015 (which included almost 1000 children from almost multiple different populations across the continent of Europe, North and south America, the genetic variants that are present on major histocompatibility complex (MHC) locus of chromosome 6 has been suggested to confer susceptibility to systemic juvenile idiopathic arthritis (sJIA) specifically on HLA-DRB1*11.
The last subtype is called the Spondyloarthropathies which describes an entity of JIA which includes inflammation of the axial skeleton, the sacroiliac joints and enthesitis (inflammation of tendon insertion). In terms of investigation, this group often tests positive for HLA-B27.
_(14781042361).jpg)
Complications
Chronic inflammation can cause a lot of damage and scarring but more importantly in this case is the production of protease and collagenase (Enzymes that degrades protein and collagen respectively) which if left untreated, will lead to the destruction of the articulating cartilage between the joint and just like the disease process in osteoarthritis, the continuous wear and tear injury of the cartilage will expose and erode the underlying bony structure.
The patient can also develop loss of function of the affected joint(s) either due to contracture, loss of joint space or bony fusion. Lastly, since the disease affects the eye, untreated uveitis can potentially lead to serious blindness.
Management
To no surprise, the treatment focuses on suppressing inflammation and at the same time, preserve or maximise the joint function, prevention of deformity and blindness.
Suppressing inflammation can be achieved by using anti-inflammatory drugs such primarily from the NSAIDs group (Acetaminophen, Celecoxib, Sodium diclofenac, etc.) Systemic corticosteroids should well be avoided unless there is recurrence and persistent symptoms or severe organ impairment is present such as in the case of Systemic-onset JIA.
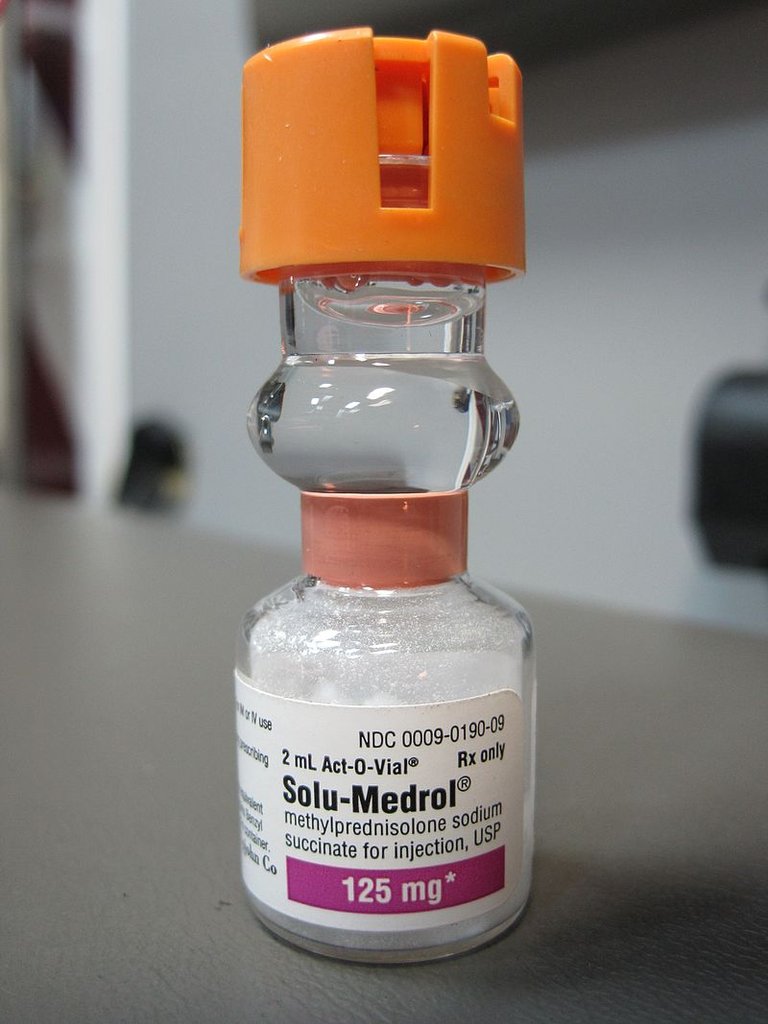
Failure to respond to Steroids (Both systemic or Intra-articular injection) will necessitate the use of DMARDS (Disease-Modifying Anti-rheumatic drugs)
In the Spondyloarthropathies group, Tumor Necrosis Factor (TNF) blockers are routinely used which includes Inflixumab and Adalimumab
Another important aspect of treatment is physiotherapy with the focus on reducing joint swelling, enhancing the joint flexibility and ensuring that contracture and gait disturbance is minimised at the same time, improve the quality of life of the patient, particularly with mobilisation. Splinting therapy may also be used to reduce pain with mobilisation.
A visit to the ophthalmologist is also indicated to rule out Uveitis as it can be asymptomatic. Should the first visit be normal, further follow up is needed to detect any development in eye symptoms.
Of course, it goes without saying that patients who are on long-term use of NSAIDs or DMARDs needes regular blood and urinary monitoring to look for toxicity and renal damage.
With that, we have reached the end of this episode, be sure to see your doctor when you managed to identify any peculiar rashes accompanied by joint pain in your children. Thank you for reading, absolutely smash that like button if you enjoyed this post or learned something Fishy from it (Pun intended). Be sure to follow me for more awesome content.
References:
Cassidy JT, Petty JE, Juvenile Idiopathic Arthritis. In: Cassidy JT, Petty RE eds. Textbook of Paediatric Rheumatology. 4th Edition. Philadephia: W.B. Saunders Company, 2011.
Marcdante KJ, RM Kliegman, Nelson Essentials of Paediatric 7th Edition, International Edition, Elsevier Inc, 2017; 305-308.
Ansell B. Rheumatic disease mimics in childhood. Curr opin Rheumatology 2000; 12 445-47.
Wallace CA, Current management in JIA. Best pract res clin Rheumatology 2006; 20: 279-300.
Waohhhh
This is really educative... I am impressed
Will love to read more of this here
Thank you so much :) That really means a lot to me, motivates me to keep making this kind of post ;)
I had rashes last month all over my armpit. Turns out it was an allergy to a whitening cream I have stopped using. My derma told me it was because that cream has mercury contents. It was horrible! I couldnt eat peanuts,seafood or anything that could worsen my allergies. I isolated myself for 1 week and glad I recovered. Great article @thethinkingdr, I can see that you are also responsive to comments on your posts. Keep it up!
Thank you so much for sharing the experience. In Malaysia, we are facing a problem of too many pseudoscience beauty products which contain harmful chemicals not certified by the ministry, one of which is of course mercury. The rule of thumb here is to only use products that are sold in the pharmacy. I have another post coming up on this series ;) My pleasure to have you reading and commenting here
Sure anytime buddy. 😉
This was a very educative and knowledge-impacting read. Thanks for sharing with us. I've written something about chewing gums as well. You could stop by on my blog and leave me a comment.
Sounds chewy, haha I shall remember to have a look at it :) Thank you for dropping by.
If I see something strange on my skin, I forget about it for a couple of days. If it is still there after that I start paying attention. How is my policy? Smart? Risky?
Oh wow, haha well I guess that's rational enough. The take home message is when there is rash with fever, that's a red flag right there.