HEADACHES
Own Image, created by @avose
Most of us have experienced headache at one time or the other and they are definitely uncomfortable and disabling. How many of these ‘not-so-familiar’ headache facts did you know?
- Most headaches are harmless and can be cured by headache medications and lying in a dark quiet room.
- Two-thirds of adults have headache at some points in their lives.
- Currently 50% of all adults are experiencing a headache.
- About 90% of headaches are primary headaches and most of these headaches are caused by tension headache.
- Worldwide, more than 12% of people have migraines and women have migraines more than men.
- Headache can be associated with nausea and vomiting especially in migraines.
- Some headaches can be associated with symptoms that mimic stroke
- Primary coital headache is a type of uncommon primary headache that occurs during sexual activity and becomes worse during orgasm.
- Primary cough headache is also a type of primary headache which occurs due to anything that increase the head pressure such as coughing, sneezing or when laughing hard. It happens suddenly and lasts for several minutes after.
Own Image, created by @avose
What then is Headache?
Headache is basically pain or ache in the head including the face and neck. This pain can be described as dull, sharp, throbbing, constant, intermittent, mild, or intense depending on the type of headache.
Classification of headaches
Headaches are classified into;
A. Primary headaches
B. Secondary headaches
Own Image, created by @avose
A] Primary Headaches
These headaches are usually benign, recurrent headaches and are not due to any underlying medical problems. While primary headaches can be discomforting and disabling, they are often harmless.
Primary headaches includes;
- Migraine
- Tension type headache
- Cluster headache
- Others
Own Image, created by @avose
1} Migraine headache.
Migraine is a complex neurovascular disorder which presents with recurrent episodes of one-sided (unilateral) headache, and can be associated with or without aura (ie visual and sensory symptoms). Migraine is generally more common in men than women and it occurs in genetically predisposed individuals.
Migraine typically presents with:
• Episodic pulsatile or throbbing headache, with moderate to severe pain that gets worse with physical activity.
• One-sided localized pain in the fronto-temporal region and around the eye
• Headache attack typically lasts for 4hours to 3 days
• Headache is dull at onset and later throbbing
• Nausea and vomiting, anorexia, food intolerance and light-headedness
• Sensitivity to light (photophobia) sound (phonophobia) and even smell.
Own Image, created by @avose
What are auras in migraine?
Auras are peculiar sensations perceived by a patient preceding the appearance of a medical condition often affecting the brain.
Aura features includes;
Auras may come before the headache attack or accompany the headache or may even occur in isolation.
They begin over 5–20 minutes and last for about 60 minutes
They are mostly visual but can also be sensory or both
• Visual auras
The most common visual symptom is the scintillating scotoma, an arc or band of absent vision with a shimmering or glittering zigzag border
Visual hallucinations
Photopsia (flashes of light)
• Sensory auras
Paraesthesias(pins and needles sensation)
• Other auras
Hemiparesis (weakness on one side of the body)
Dysphasias (language disorder)
Olfactory and gustatory hallucinations
Distortion of body parts such as tongue swelling
yawning, irritability, neck pain, food cravings, burst of energy, or fatigue.
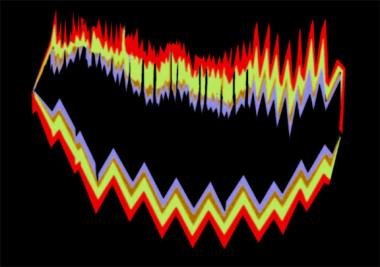
source
image showing visual auras
What causes Migraine?
The definitive cause of migraine still remains unknown, although some triggers has been implicated
Migraine triggers includes;
• Stress and relaxation after stress
• Hormonal changes: estrogen fluctuations during menstrual cycle, pregnancy and menopause
• Sleep changes: lack of or unaccustomed excess
• Sensory stimulation: sun glare, increased screen time, flickering lights, strong smells including certain perfumes and smokes, loud sounds
• Trauma
• Missing a meal (hypoglycaemia)
• Foods and drinks including cheese, and salty processed foods caffeine in coffee and chocolate, alcohol in red wine
• Food additives: monosodium glutamate and aspartame
• Exercise: intense physical exertion and also sexual activity can provoke migraines
• Excess heat and dehydration
• Drugs: vasodilators such as nitroglycerine, oral contraceptive pills and hormone replacement therapy
• Changes in weather or barometric pressure, e.g thunderstorm
Own Image, created by @avose
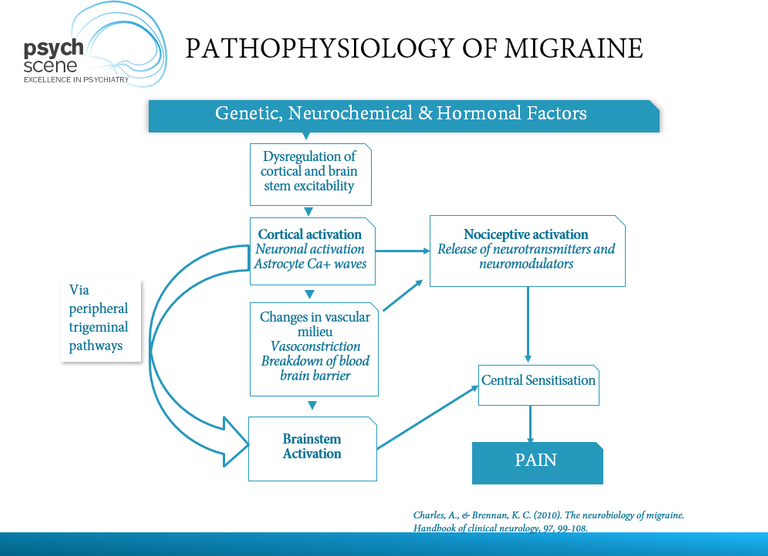
Pathophysiology of Migraine
How can Migraines be Treated?
The treatment of migraine can be broadly divided into two main categories
• Non-pharmacologic: which invoves lifestyle modifications to avoid the triggers
• Pharmacologic which involves the use of medications. Medications used to treat migraines are divided into 3
- Acute symptomatic treatment: This makes use of simple analgesics with anti-emetics such as
Aspirin 900-1200mg (dissolved) + IV metoclopramide 10mg or domperidone 10-20mg
Alternative drugs: such as Paracetamol 1000mg and NSAIDS e.g ibuprofen, naproxen, diclofenac - Abortive or definitive treatment: the drug of choice in the treatment of migraine is a class of drug called Triptans, examples of drugs in this class are-sumatriptan, zolmitriptan, naratriptan, rizatriptan, eleptriptan, almotriptan, frovatriptan.All drugs of this class have high efficacy and they work best when taken early but not during the aura phase. There is up to 70% response within 2 hours and 40% being pain free at 2 hours. Headache reoccurrence within 12-24 hours occurs in 30%. If no response, try another triptan.
- Prophylactic or preventive treatment: indications for this treatment includes >2 attacks /month and One prolonged attack affecting lifestyle.
Drugs used includes
Beta blockers: selective e.g atenolol, metoprolol; non-selective e.g propranolol, timolol, nadolol
5-HT2 antagonists: pizotifen, cyproheptadine, methysergide
Anti-epileptic drugs: sodium valproate, topiramate, gabapentin.
2} Tension-type headaches
What are tension headaches?
These headaches are often called muscle-contraction headaches. It is a headache without features. The pain is diffuse and severity is mild to moderate which is described as a tight-band around the head. It is the most common type of headache.
Features of tension headaches
• Headaches are generally bilateral and diffuse in location.
• They are mild to moderate constant or intermittent lasting hours to days
• Described as tightness or pressure
• Does not interfere with activity
• Not associated with other features like sensitivity to light, noise or nausea and vomiting.
Pathophysiology of tension headache
It is due to sustained contraction of the craniocervical muscles (muscles in the head and neck) caused by such trivial issues as stress, fatigue and lack of sleep.

Own Image, created by @avose
Treatment of tension headaches
Treatment of tension headache includes;
- Abortive treatment: which involves the use of simple analgesics not more than 2-3 days/week toprevent medication misuse headache
- Preventive treatment: indications includes troublesome or disabling headaches despite abortive treatmentsand Headache frequency exceeds twice a week on a regular basis.Drugs for preventive treatment includes Amitriptylin, Imipramine and Doxepine.
3} Cluster headaches
This type of headache is the least common type of Primary headache and can be described as “suicide” headache because of its severity. Cluster headache is also called migranous neuralgia or alarm clock headache.
Features of cluster headache
• Excruciatingly recurrent severe unilateral pain which occurs around the eye.
• Lasts 15-180 minutes (usually 45-90 mins)
• Frequency may range from 1 every other day to 8/day
• Abrupt onset and cessation
• Restlessness/agitation during attack causing patients to pace or rock in order to relieve pain
• Associated autonomic features- lacrimation (tears in the eye), nasal congestion, rhinorrhoea (nasal congestion), forehead sweating, miosis, ptosis, eyelid oedema
Causes of cluster headache
The exact cause of cluster headache is unknown but a few factors has been implicated
• Nerves: the trigeminal and facial nerve cause the associated autonomic feature seen in cluster headache such as lacrimation, rhinorrhoea, miosis and ptosis
• Genetics : studies has shown that cluster headache runs in some families and that people with a first degree relative who has cluster headache are about 15-50 times likely to develop this headache themselves.
• Tobacco smoking : 65% or more of persons with cluster headaches are either smokers or have smoked at a point in their lives.
Pathophysiology of Cluster Headache
This mechanism is poorly understood
Treatment of Cluster Headaches
There are two approach to treat cluster headaches
- Acute attack
• Sumatriptan: 6 mg subcutaneously
• 100% oxygen: 8-12L/min for 20 min
• Lidocaine: 20-60 mg of 4-6% topical solutioninstilled intranasally. - Preventive treatments
A. Short term: prednisolone, methysergide, ergotamine
B. Long-term: lithium, verapamil

Own Image, created by @avose
Own Image, created by @avose
4} Other Primary Headaches
• Primary cough headache
• Primary exertional headache
• Primary coital headache
• Primary stabbing headache (ice pick, jab-and-jolts headache)
• Primary thunderclap
• Hypnic headache
• Hemicrania continua
• New persistent daily headaches

Own Image, created by @avose
B] Secondary Headaches
Secondary headaches are caused by an underlying systemic disease somewhere other than the head and neck such as infections, head injury, vascular disorders, or tumors. Secondary headaches can be dangerous and can be associated with certain "red flags" or warning signs.
A person with secondary headache must have;
• A disorder known to cause the headache.
• Headaches that occur in close temporal relationship to the disorder/ and or there is no other causation.
• Headaches that are reduced or remit within 3 months spontaneously or after the treatment of the cause.
Features that might suggest a secondary headache
• Age >50
• Significant change in headache pattern for <2 years
• Pain in posterior head or neck
• Additional medical symptoms
• Additional neurologic symptoms
• Abnormal physical or neurological findings
Causes of Secondary headaches
- Head trauma
• Acute post-traumatic headache
• Chronic post-traumatic headache - Infection
• Intracranial infection
• Systemic infection
• HIV/AIDS - Cranial or cervical vascular disorder
• Ischaemic stroke or TIA (Transient Ischaemic Attack)
• Non -traumatic SAH (Sub-Arachnoid Haemorrhage)
• Unruptured vascular malformation
• Cerebral venous thrombosis - Non-vascular intracranial disorder
• High CSF pressure (Cerebro-Spinal Fluid)
• Low CSF pressure (e.g post lumbar puncture)
• Non-infectious inflammatory disease
• Epileptic seizure
• Intracranial tumor - Substance use or its withdrawal
• Acute substance use or exposure
• Substance withdrawal
• Medication-overuse headache (MOH)
• Side-effect of chronic medication - Disorders of homeostasis
• Hypoxia/hypercapnia
• Hypertension
• Dialysis headaches
• Hypothyroidism
• Fasting - Psychiatric disorder
• Somatization disorder
• Psycotic disorder - Disorders of craniofacial structures
• Disorder of cranial bone
• Disorder of neck
• Disorder of eyes
• Disorder of ears
• Disorder of paranasal sinuses
• Disorder of teeth, jaw or related structures - Cranial neuralgias and central causes of facial pain.
• Trigeminal neuralgia
• Glossopharyngeal neuralgia
• Occipital neuralgia
• Neck-tongue syndrome
• External compression headache
Own Image, created by @avose
Treatment of Secondary Headaches
Treatment of secondary headache usually involves treating the underlying cause, after which the headache should resolve.
References
1] Clinch C. Chapter 28. Evaluation & Management of Headache - CURRENT Diagnosis & Treatment in Family Medicine, Third Edition (Lange Current Series): Jeannette E. South-Paul, Samuel C. Matheny, Evelyn L. Lewis. McGraw-Hill. 2011. ISBN 9780071624367.
2] http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/neurology/headache-syndromes/
3] https://emedicine.medscape.com/article/1142556-overview
4] https://www.medicinenet.com/headache/article.htm
5] https://www.mayoclinic.org/diseases-conditions/tension-headache/symptoms-causes/syc-20353977#:~:text=A%20tension%20headache%20is%20generally,aren't%20well%2Dunderstood.
Interesting read. Thanks!
Thank you so much!
What an awesome post!
Thank you
Please are you a medical practitioner?
Yes I am🙂
Oh sorry u mentioned it before. Wow amazing to have you here your post is awesome. Check out natural medicine community too they share nice natural medicine stuff and I think there will be a lot of content for u to relate with there. Nice to see you post again, looking forward to your next posts for us. Cheers
Thank you so much! I'll check it asap
@tipu curate
Upvoted 👌 (Mana: 14/21)
Good read dear.. keep it up
Thank you
This is a long one and a really good effort. The formatting of the post can be much better, I am sure with time you will improve on this.
I am a bit concerned by your images, did you make them from the scratch or you modify images from someone else? This is quite important so as to ensure that there are no copyright issues with your images. Feel free to tag me when you respond to this comment.
Thank you so much @gentleshaid. I'll work on my formatting. The images are original images made by me using open source clip arts.
Good post and nice information friends 😁
Thank you🙌
Your Welcome friends 😊
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider supporting our funding proposal, approving our witness (@stem.witness) or delegating to the @stemsocial account (for some ROI).
Thanks for using the STEMsocial app and including @stemsocial as a beneficiary, which give you stronger support.
Congratulations @avose! You have completed the following achievement on the Hive blockchain and have been rewarded with new badge(s) :
You can view your badges on your board And compare to others on the Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPDo not miss the last post from @hivebuzz:
Support the HiveBuzz project. Vote for our proposal!
What about a young person getting numb feeling in the front cortex, but real heaviness in the back of the head...... it moves the side we move. Its kind of a metal ball moving around our head and hitting hard on the sides? Have you ever felt that way?
Applied even ice in the neck as in a video, nothing happened. Peppermint diffuse also failed in the remedy. I am a frequent mediator.
Sorry dear....
That could be a type of secondary headache and in order to diagnose you need to see a doctor
Thanks for sharing these great information about headaches and its treatment. Cheers!